Disease prevention and bone health: 5 Things people with diabetes need to know about osteoporosis
11/22/2019 / By Grace Olson
Managing diabetes is already difficult, but unbeknownst to many, it also increases the risk of other diseases. Diabetes and some of its treatments can weaken the bones and increase the possibility of fractures. Without proper control, diabetics may develop osteoporosis.
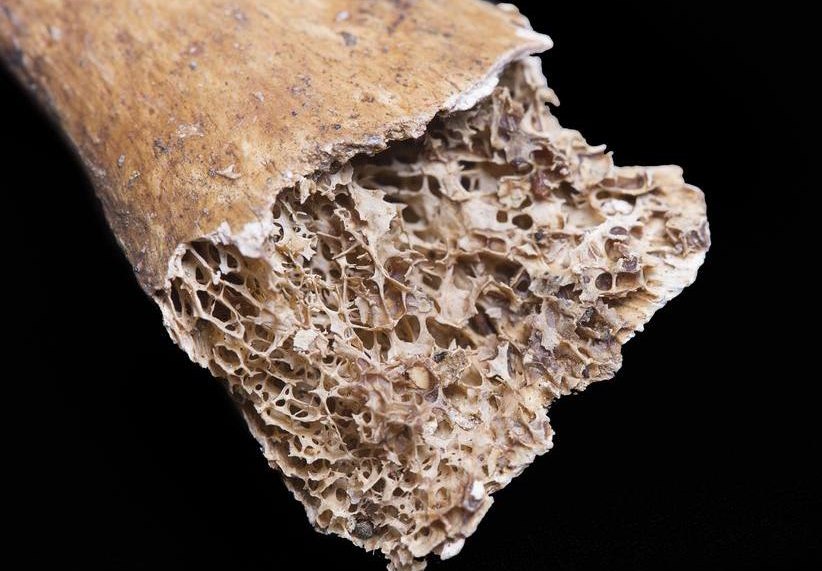
People with osteoporosis lose bone density, making them more likely to sustain fractures. When bones break, especially the hip bone, it can have lasting effects on a person’s life. Like diabetes, there is no cure for osteoporosis.
Here are some things you need to know about the link between diabetes and osteoporosis:
1. Maintaining HbA1C levels is crucial to bone health
HbA1C refers to glycated hemoglobin, which are red blood cells with glucose molecules attached to them. High HbA1C is an indicator of diabetes. It also means an increased risk of osteoporosis.
HbA1C activates osteoclasts, the cells that break down bones. HbA1C also makes bones more prone to fractures by sticking to the collagen fibers that keep bone minerals together. This makes the fibers stiff and results in weak bones.
2. Sudden drops in blood sugar levels trigger inflammation
The primary focus of diabetes treatments and management strategies is to lower blood sugar levels. However, this often leads to hypoglycemia. Drastic changes in blood sugar levels also causes inflammation.
According to studies, hypoglycemia is associated with a rise in inflammatory compounds, which causes abnormalities in blood coagulation and blood vessel injuries. This inflammation can negatively affect the heart, the eyes, the nerves, and the bones. For people with diabetes, this can cause blindness and increase their risk of fractures.
3. GLP-1 inhibitors affect bone regeneration
Glucagon-like peptide or GLP-1 inhibitors are medications used to manage insulin. But while they stop blood sugar levels from dipping too low, GLP-1 inhibitors also affect the development of osteoblasts and osteoclasts.
Osteoblasts are bone-building cells while osteoclasts are bone-destructive cells. Both are crucial for bone regeneration and maintenace. GLP, the protein target of GLP-1 inhibitors, regulates the development of osteoblasts and osteoclasts. By inhibiting GLP, GLP-1 inhibitors interfere with the bones’ ability to absorb minerals and slow down bone regeneration.
4. Thiazolidinediones may cause fat to be stored in bones
Thiazolidinediones (TZDs) used to be popular medications for diabetes back in the 1990s. But it was soon discovered that these drugs activate the nuclear hormone receptor PPAR-gamma, which helps fat cells store sugar.
Not only that, PPAR-gamma also causes stem cells inside the bones — ones that are intended to become bone cells — to turn into fat cells. The presence of fat in bones results in fractures. Moreover, these fats cannot be removed. Even after diabetics had stopped taking TZDs, their high risk for developing broken bones still remained.
5. Not all functional foods are good for Type 2 diabetes
Most functional foods are great for overall health, including bone health. However, there is one functional food that is not good for people with Type 2 diabetes: whey protein.
Whey protein is commonly added to smoothies to aid in muscle recovery. However, it also promotes the production of insulin, which people with Type 2 diabetes — who are already producing too much insulin — don’t need. Consuming whey protein only aggravates their insulin resistance.
Ways to prevent and manage osteoporosis
Osteoporosis has no symptoms. In fact, people only discover that they have osteoporosis when they experience joint pain or sustain bone fractures. Because people with diabetes are more prone to developing this bone disease, they need to be extra careful. To maintain healthy bones, try the following tips:
- Eat foods rich in calcium and vitamin D. The bones need calcium to stay strong, but for the body to absorb calcium effectively, it needs vitamin D. Foods rich in calcium include green leafy vegetables, soybeans, and some fresh fish. Meanwhile, vitamin D can be obtained naturally through sun exposure or by taking supplements and eating fortified food products.
- Exercise. Bones respond well to weight-bearing and resistance exercises. Regular exercise enhances balance and flexibility, thus decreasing the chances of falling and developing bone fractures.
- Stop smoking and drinking alcohol. Smoking and alcohol drinking have negative effects on bone health. Smoking prevents calcium absorption while alcohol intake increases bone loss and the risk of fractures.
- Take bone density tests. Talk to your health care provider about taking bone density tests. These help diagnose osteoporosis early on before you sustain any bone fracture. (Related: Osteoporosis remains undiagnosed in millions of Americans; here’s how to beat the disease with nutrition, exercise and sunlight.)
Having diabetes increases your risk of many conditions, including osteoporosis. But knowing how to properly manage diabetes and maintain healthy bones is the best way to prevent developing this complication.
Sources include:
Tagged Under: blood sugar, bone fractures, bone health, exercise, inflammation, insulin resistance, nutrients, osteoporosis, Prescription drugs, prevention, stopsmoking, Type 2 Diabetes, vitamin D
RECENT NEWS & ARTICLES
COPYRIGHT © 2017 NUTRIENTS NEWS